DEFINITION So many patients ask, “What is Lupus?” Really, lupus is a very complicated diseaes, so, for educational purposes, I am giving you this written information. Lupus is a chronic, autoimmune disease which causes inflammation of various parts of the body, especially the skin, joints, blood and kidneys. The body's immune system normally makes proteins called antibodies to protect the body against viruses, bacteria and other foreign materials. These foreign materials are called antigens. In an autoimmune disorder such as lupus, the immune system loses its ability to tell the difference between foreign substances (antigens) and its own cells and tissues. The immune system then makes antibodies directed against "self." These antibodies, called "auto-antibodies," react with the "self" antigens to form immune complexes. The immune complexes build up in the tissues and can cause inflammation, injury to tissues, and pain. More people have lupus than AIDS, cerebral palsy, multiple sclerosis, sickle-cell anemia and cystic fibrosis combined. LFA market research data show that between 1,400,000 and 2,000,000 people reported to have been diagnosed with lupus. (Study conducted by Bruskin/Goldring Research, 1994.) For most people, lupus is a mild disease affecting only a few organs. For others, it may cause serious and even life-threatening problems. Thousands of Americans die each year from lupus-related complications.
History of Lupus Lupus has been known to physicians since 1828 when it was first described by the French dermatologist, Biett. Early studies were simply descriptions of the disease, with emphasis on the skin chances. A dermatologist named Kaposi, 45 years later, noted that some patients with LE skin lesions showed signs that the affected internal organs. In the 1890s, sir William Osler, a famed American physician, observed that systemic LE could affect internal organs without the occurrence of skin changes. In 1948, Dr. Malcolm Hargraves of the Mayo Clinic described the LE cell, a particular cell found in the blood of patients with SLE. His discovery has enabled physicians to identify many more cases of LE by using a simple blood test. As a result, during the succeeding years the number of SLE cases diagnosed has steadily risen. Since 1954, various unusual proteins (antibodies) that act against the patient's own tissues have been found to be associated with SLE. Detection of these abnormal proteins has been used to develop more sensitive tests for systemic LE (anti nuclear antibody test). The presence of these antibodies may be the result of factors other than SLE.
TYPES OF LUPUS There are three types of lupus: discoid, systemic, and drug-induced. Discoid lupus is always limited to the skin. It is identified by a rash that may appear on the face, neck and scalp. Discoid lupus is diagnosed by examining a biopsy of the rash. In discoid lupus the biopsy will show abnormalities that are not found in skin without the rash. Discoid lupus does not generally involve the body's internal organs. Therefore, the ANA test, a blood test used to detect systemic lupus, may be negative in patients with discoid lupus. However, in a large number of patients with discoid lupus, the ANA test is positive, but at a low level or "titer." In approximately 10 percent of the people with lupus, discoid lupus can evolve into the systemic form of the disease, which can affect almost any organ or system of the body. This cannot be predicted or prevented. Treatment of discoid lupus will not prevent its progression to the systemic form. Individuals who progress to the systemic form probably had systemic lupus at the outset, with the discoid rash as their main symptom. Systemic lupus is usually more severe than discoid lupus, and can affect almost any organ or system of the body. For some people, only the skin and joints will be involved. In others, the joints, lungs, kidneys, blood or other organs and/or tissues may be affected. Generally, no two people with systemic lupus will have identical symptoms. Systemic lupus may include periods in which few, if any, symptoms are evident (remission) and other times when the disease becomes more active (flare). Most often when people mention "lupus," they are referring to the systemic form of the disease. Drug-induced lupus occurs after the use of certain prescribed drugs. The symptoms of drug-induced lupus are similar to those of systemic lupus. The drugs most commonly connected with drug-induced lupus are hydralazine (used to treat high blood pressure or hypertension) and procainamide (used to treat irregular heart rhythms). However, not everyone who takes these drugs will develop drug-induced lupus. Only about 4 percent of the people who take these drugs will develop the antibodies suggestive of lupus. Of those 4 percent, only an extremely small number will develop overt drug-induced lupus. The symptoms usually fade when the medications are discontinued. Although drug-induced lupus and discoid lupus share features of systemic lupus, the rest of this brochure primarily discusses systemic lupus. CAUSE The cause(s) of lupus is unknown, but environmental and genetic factors are involved. While scientists believe there is a genetic predisposition to the disease, it is known that environmental factors also play a critical role in triggering lupus. Some of the environmental factors that may trigger the disease are infections, antibiotics (especially those in the sulfa and penicillin groups), ultraviolet light, extreme stress, and certain drugs. Although lupus is known to occur within families, there is no known gene or genes which are thought to cause the illness. Only 10 percent of lupus patients will have a close relative (parent or sibling) who already has or may develop lupus. Statistics show that only about 5% of the children born to individuals with lupus will develop the illness. Lupus is often called a "woman's disease" despite the fact that many men are affected. Lupus can occur at any age, and in either sex, although it occurs 10-15 times more frequently among adult females than among adult males. The symptoms of the disease are the same in men and women. People of African, American Indian, and Asian origin are thought to develop the disease more frequently than Caucasian women, but the studies that led to this result are small and need corroboration. Hormonal factors may explain why lupus occurs more frequently in females than in males. The increase of disease symptoms before menstrual periods and/or during pregnancy support the belief that hormones, particularly estrogen, may be involved. However, the exact hormonal reason for the greater prevalence of lupus in women, and the cyclic increase in symptoms, is unknown. PREGNANCY AND LUPUS A question of concern to many families is whether or not a young woman with lupus should risk becoming pregnant. The current general view is that there is no absolute reason why a woman with lupus should not get pregnant, unless she has moderate to severe organ involvement (i.e., central nervous system, kidney, or heart and lungs) which would place the mother at risk. However, there is some increased risk of disease activity during or immediately (3 to 4 weeks) after pregnancy. If a person is monitored carefully, the danger can be minimized. A pregnant woman with lupus should be closely followed by both her obstetrician and her "lupus doctor."
SYMPTOMS OF LUPUS Although lupus can affect any part of the body, most people experience symptoms in only a few organs. The following lists the most common symptoms of people with lupus.
SYMPTOMS OF LUPUS Achy joints (arthralgia) 95% Fever over 100 degrees F (38 degrees C) 90% Arthritis (swollen joints) 90% Prolonged or extreme fatigue 81% Skin Rashes 74% Anemia 71% Kidney Involvement 50% Pain in the chest on deep breathing (pleurisy) 45% Butterfly-shaped rash across the cheeks and nose 42% Sun or light sensitivity (photosensitivity) 30% Hair loss 27% Raynaud's phenomenon (fingers turning white and/or blue in the cold) 17% Seizures 15% Mouth or nose ulcers 12%
DIAGNOSIS Because many lupus symptoms mimic other illnesses, are sometimes vague and may come and go, lupus can be difficult to diagnose. Diagnosis is usually made by a careful review of a person's entire medical history coupled with an analysis of the results obtained in routine laboratory tests and some specialized tests related to immune status. Currently, there is no single laboratory test that can determine whether a person has lupus or not. To assist the physician in the diagnosis of lupus, the American Rheumatism Association issued a list of 11 symptoms or signs that help distinguish lupus from other diseases . A person should have four or more of these symptoms to suspect lupus. The symptoms do not all have to occur at the same time.
THE ELEVEN CRITERIA USED FOR THE DIAGNOSIS OF LUPUS Malar Rash- Rash over the cheeks. Discoid Rash- Red raised patches. Photosensitivity- Reaction to sunlight, resulting in the development of or increase in skin rash. Oral Ulcers- Ulcers in the nose or mouth, usually painless. Arthritis- Nonerosive arthritis involving two or more peripheral joints (arthritis in which the bones around the joints do not become destroyed). Serositis- Pleuritis or pericarditis. Renal Disorder- Excessive protein in the urine (greater than 0.5 gm/day or 3+ on test sticks) and/or cellular casts (abnormal elements the urine, derived from red and/or white cells and/or kidney tubule cells). Neurologic Seizures- (convulsions) and/or psychosis in the absence of drugs or metabolic disturbances which are known to cause such effects. Hematologic Disorder- Hemolytic anemia or leukopenia (white blood count below 4,000 cells per cubic millimeter) or lymphopenia (less than 1,500 lymphocytes per cubic millimeter) or thrombocytopenia (less than 100,000 platelets per cubic millimeter). The leukopenia and lymphopenia must be detected on two or more occasions. The thrombocytopenia must be detected in the absence of drugs known to induce it. Immunologic Disorder- Positive LE prep test, positive anti-DNA test, positive anti-Sm test or false positive syphilis test (VDRL). Antinuclear Antibody Positive test for antinuclear antibodies (ANA) in the absence of drugs known to induce it.
LABORATORY TESTS USED IN THE DIAGNOSIS OF LUPUS: The first laboratory test ever devised was the LE (lupus erythematosus) cell test. When the test is repeated many times, it is eventually positive in about 90 percent of the people with systemic lupus. Unfortunately, the LE cell test is not specific for systemic lupus (despite the official-sounding name). The test can also be positive in up to 20 percent of the people with rheumatoid arthritis, in some patients with other rheumatic conditions like Sjogren's syndrome or scleroderma, in patients with liver disease, and in persons taking certain drugs (such as procainamide, hydralazine, and others). The immunofluorescent antinuclear antibody (ANA, or FANA) test is more specific for lupus than the LE cell prep test. The ANA test is positive in virtually all people with systemic lupus, and is the best diagnostic test for systemic lupus currently available. If the test is negative, the patient will likely not have systemic lupus. On the other hand, a positive ANA, by itself, is not diagnostic of lupus since the test may also be positive in 1. individuals with other connective tissue diseases; 2. individuals without symptoms; 3. patients being treated with certain drugs, including procainamide, hydralazine, isoniazid, and chlorpromazine; 4. individuals with conditions other than lupus, such as scleroderma, rheumatoid arthritis, infectious mononucleosis and other chronic infectious diseases such as lepromatous leprosy, subacute bacterial endocarditis, malaria, etc., and liver disease. ANA test reports include a titer. The titer indicates how many times an individual's blood must be diluted to get a sample free of anti-nuclear antibodies. Thus, a titer of 1:640 shows a greater concentration of anti-nuclear antibodies than a titer of 1:320 or 1:160. The titer is always highest in people with lupus. Patients with active lupus have ANA tests that are very high in titer. Laboratory tests which measure complement levels in the blood are also of some value. Complement is a blood protein that, with antibodies, destroys bacteria. It is an "amplifier" of immune function. If the total blood complement level is low, or the C3 or C4 complement values are low, and the person also has a positive ANA, some weight is added to the diagnosis of lupus. Low C3 and C4 complement levels in individuals with positive ANA test results may also be indicative of lupus kidney disease. New tests of individual antigen antibody reactions have been developed which are very helpful in the diagnosis of SLE. These include the anti-DNA antibody test, the anti-Sm antibody test, the anti-RNP antibody test, the anti-Ro antibody test, and tests which measure serum complement levels. These tests can also be further explained by your physician. Laboratory tests are most useful when one remembers the following information. If an individual has signs and symptoms supporting the diagnosis of lupus (e.g., at least four of the American Rheumatism Association criteria), a positive ANA confirms the diagnosis and no further testing is necessary. If a person has only two or three of the American Rheumatism Association criteria, then a positive ANA supports the diagnosis. In these cases, unless more specific tests are positive (e.g., anti-DNA, anti-Sm, anti-Ro) the diagnosis of lupus is uncertain until more clinical findings develop or other more specific blood tests, as cited above, become positive. Physicians will sometimes also perform skin biopsies of both the individual's rashes and his or her normal skin. These biopsies can help diagnose systemic lupus in about 75 percent of patients. The interpretation of all these positive or negative tests, and their relationship to symptoms, is frequently difficult. A test may be positive one time and negative another time, reflecting the relative activity of the disease or other variables. When questions cannot be resolved, consult an expert in lupus. When someone has many symptoms and signs of lupus and has positive tests for lupus, physicians have little problem making a correct diagnosis and initiating treatment. However, a more common problem occurs when an individual has vague, seemingly unrelated symptoms of achy joints, fever, fatigue, or pains. Some doctors may think the person is neurotic. Others may try different drugs in the hope of suppressing the symptoms. Fortunately, with growing awareness of lupus, an increasing number of physicians will consider the possibility of lupus in the diagnosis. A patient can help the doctor by being open and honest. A healthy dialogue between patient and doctor results in better medical care, not only for people with lupus, but for anyone seeking medical treatment. To whom should a person go for a diagnosis of lupus? Most individuals usually seek the help of their family doctor first, and this is often sufficient. However, when unresolved questions arise or complications develop, another opinion from a specialist may be advisable. The choice of specialist depends on the problem. For example, you would see a nephrologist for a kidney problem or a dermatologist for a skin problem. Most often, a rheumatologist or clinical immunologist specializing in lupus is recommended. Referrals can be made through your family doctor, the local medical society, or the local Lupus Foundation chapter.
FLARES: WHAT TRIGGERS LUPUS? What triggers an attack of lupus in a susceptible person? Scientists have noted common features in many lupus patients. In some, exposure to the sun causes sudden development of a rash and then possibly other symptoms. In others an infection, perhaps a cold or a more serious infection, does not get better, and then complications arise. These complications may be the first signs of lupus. In still other cases, a drug taken for some illness produces the signaling symptoms. In some women, the first symptoms and signs develop during pregnancy. In others, they appear soon after delivery. Many people cannot remember or identify any specific factor. Obviously, many seemingly unrelated factors can trigger the onset of the disease.
TREATMENT For the vast majority of people with lupus, effective treatment can minimize symptoms, reduce inflammation, and maintain normal bodily functions. Preventive measures can reduce the risk of flares. For photosensitive patients, avoidance of (excessive) sun exposure and/or the regular application of sun screens will usually prevent rashes. Regular exercise helps prevent muscle weakness and fatigue. Immunization protects against specific infections. Support groups, counseling, talking to family members, friends, and physicians can help alleviate the effects of stress. Needless to say, negative habits are hazardous to people with lupus. These include smoking, excessive consumption of alcohol, too much or too little of prescribed medication, or postponing regular medical checkups. Treatment approaches are based on the specific needs and symptoms of each person. Because the characteristics and course of lupus may vary significantly among people, it is important to emphasize that a thorough medical evaluation and ongoing medical supervision are essential to ensure proper diagnosis and treatment. Medications are often prescribed for people with lupus, depending on which organ(s) are involved, and the severity of involvement. Effective patient-physician discussions regarding the selection of medication, its possible side effects, and any changes in doses are vital. Commonly prescribed medications include Nonsteroidal Anti-Inflammatory Drugs (NSAIDs): These medications are prescribed for a variety of rheumatic diseases, including lupus. The compounds include acetylsalicylic acid (e.g., aspirin), ibuprofen (Motrin), naproxen (Naprosyn), indomethacin (Indocin), sulindac (Clinoril), tolmetin (Tolectin), and a large number of others. These drugs are usually recommended for muscle and joint pain, and arthritis. Aspirin may cause stomach upsets for some people. This effect can be minimized by taking them with meals, milk, or antacids. The other NSAIDs work in the same way as aspirin, but tend to be less irritating to the stomach than aspirin, and often require fewer pills per day to have the same effect as aspirin. Acetaminophen: Acetaminophen (e.g., Tylenol) is a mild analgesic that can often be used for pain. It has the advantage of less stomach irritation than aspirin, but it is not nearly as effective at suppressing inflammation as aspirin. Corticosteroids: Corticosteroids (steroids) are hormones that have anti-inflammatory and immunoregulatory properties. They are normally produced in small quantities by the adrenal gland. This hormone controls a variety of metabolic functions in the body. Synthetically produced corticosteroids are used to reduce inflammation and suppress activity of the immune system. The most commonly prescribed drug of this type is prednisone. Because steroids have a variety of side effects, the dose has to be regulated to maximize the beneficial anti-immune/anti-inflammatory effects and minimize the negative side effects. Side effects occur more frequently when steroids are taken over long periods of time at high doses (for example, 60 milligrams of prednisone taken daily for periods of more than one month). Such side effects include weight gain, a round face, acne, easy bruising, "thinning" of the bones (osteoporosis), high blood pressure, cataracts, onset of diabetes, increased risk of infection and stomach ulcers. Anti-malarials: Chloroquine (Aralen) or hydroxychloroquine (Plaquenil), commonly used in the treatment of malaria, may also be very useful in some individuals with lupus. They are most often prescribed for skin and joint symptoms of lupus. It may take months before these drugs demonstrate a beneficial effect. Side effects are rare, and consist of occasional diarrhea or rashes. Some anti-malarial drugs, such as quinine and chloroquine, can affect the eyes. Therefore, it is important to see an eye doctor (ophthalmologist) regularly. The manufacturer suggests an eye exam before starting the drug and one exam every six months thereafter. However your physician might suggest a yearly exam is sufficient. Cytotoxic Drugs: Azathioprine (Imuran) and cyclophosphamide (Cytoxan) are in a group of agents known as cytotoxic or immunosuppressive drugs. These drugs act in a similar manner to the corticosteroid drugs in that they suppress inflammation and tend to suppress the immune system. The side effects of these drugs include anemia, low white blood cell count, and increased risk of infection. Their use may also predispose an individual to developing cancer. People with lupus should learn to recognize early symptoms of disease activity. In that way they can help the physician know when a change in therapy is needed. Regular monitoring of the disease by laboratory tests can be valuable because noticeable symptoms may occur only after the disease has significantly flared. Changes in blood test results may indicate the disease is becoming active even before the patient develops symptoms of a flare. Generally, it seems that the earlier such flares are detected, the more easily they can be controlled. Also, early treatment may decrease the chance of permanent tissue or organ damage and reduce the time one must remain on high doses of drugs.
NUTRITION AND DIET Although much is still not known about the nutritional factors in many kinds of disease, no one questions the necessity of a well-balanced diet. Fad diets, advocating an excess or an exclusion of certain types of foods, are much more likely to be detrimental than beneficial in any disease, including lupus. Scientists have shown that both antibodies and other cells of the immune system may be adversely affected by nutritional deficiencies or imbalances. Thus, significant deviations from a balanced diet may have profound effects on a network as complex as the immune system. There have been suggestions about various foods and the treatment of lupus. One example is fish oil. However, these diets have been used only in animals with limited success and should not become the mainstay of a person's diet.
PROGNOSIS The idea that lupus is generally a fatal disease is one of the gravest misconceptions about this illness. In fact, the prognosis of lupus is much better than ever before. Today, with early diagnosis and current methods of therapy, 80-90 percent of people with lupus can look forward to a normal lifespan if they follow the instructions of their physician, take their medication(s) as prescribed, and know when to seek help for unexpected side-effects of a medication or a new manifestation of their lupus. Although some people with lupus have severe recurrent attacks and are frequently hospitalized, most people with lupus rarely require hospitalization. There are many lupus patients who never have to be hospitalized, especially if they are careful and follow their physician's instructions. New research brings unexpected findings each year. The progress made in treatment and diagnosis during the last decade has been greater than that made over the past 100 years. It is therefore a sensible idea to maintain control of a disease that tomorrow may be curable.
THE LUPUS FOUNDATION OF AMERICA The Lupus Foundation of America (LFA) was incorporated as a nonprofit health agency in 1977. The purpose of the LFA is to assist local chapters in their efforts to provide supportive services to individuals living with lupus, to educate the public about lupus, and to support research into the cause and cure of lupus. Last year over 200,000 people received service from the LFA and its chapters. Since its establishment the Lupus Foundation has remained a grassroots, volunteer driven organization. Volunteers, through an extensive network of over 500 constituent chapters, branches, support groups and International Associated groups, provide the majority of services which link the Lupus Foundation to thousands of lupus patients and their families. Last year LFA volunteers contributed over 375,000 hours of service at the local and national levels. The Lupus Foundation of America is the largest lupus group in the world with nearly 46,000 members in 98 chapters throughout the U.S. Thousands of others are associated with the LFA through the 73 International Associated Groups in 37 countries worldwide. The LFA and its chapters contributed more than $1,000,000 for lupus research in the past two years. The LFA sets standards and provides direction and general support to its chapters, leading the efforts to operate a patient-oriented, nonprofit, voluntary health agency in an ethical and professional manner. The LFA has developed specific services and programs to provide chapters with assistance in meeting patient's needs and organizational goals. These include chapter support, volunteer leadership training, research, patient education programs, public awareness activities, professional education, advocacy, and resource development. For more information about various aspects of lupus, contact the Lupus Foundation of America.
SKIN DISEASE IN LUPUS Skin disease is very common in lupus erythematosus. It ranks second only to arthritis in frequency of occurrence. Approximately 20% of people with systemic lupus erythematosus (SLE) will have ring-shaped or coin-shaped, scarring lesions as the initial symptom of their disease. In addition, it has been estimated that as many as 60-65% of people with SLE will develop skin rashes or lesions at some time during the course of their illness. However, with the use of oral steroids (prednisone), and anti-malarial drugs (hydroxychloroquine, or Plaquenil), the occurrence of these skin lesions is now less frequent. The skin rashes and lesions of lupus erythematosus can be divided into those that are specific to lupus and those that can occur in other diseases as well as lupus (non-specific lesions). There are two specific lesions associated with lupus erythematosus: discoid lesions (characteristic of discoid lupus erythematosus), and coin-shaped, non-scarring lesions (characteristic of subacute cutaneous lupus erythematosus).
DISCOID LESIONS The term discoid is a very confusing term which, unfortunately, is inappropriately used by many people, including physicians. The term discoid simply means coin-shaped. The scarring coin-shaped lupus lesion commonly seen on areas of the skin that are exposed to light has been termed discoid lupus erythematosus. This term refers only to the description of the lupus lesion on the skin and should not be used to distinguish cutaneous lupus from systemic lupus erythematosus. A physician cannot determine whether or not a discoid lupus lesion on the skin is occurring in the presence or absence of systemic features just by examining the shape of the lesion. This can only be done by taking a complete history and physical examination and interpreting the results of appropriate blood tests. What is the relationship between discoid and systemic lupus erythematosus? This is a common question. Lupus erythematosus should be viewed as a continuum of a spectrum of the disease. At one end of the spectrum, in its most mild form, it is characterized by coin-shaped, scarring skin lesions which we term discoid lesions. At the other end of the spectrum are those systemic lupus erythematosus patients who have no skin lesions, but have systemic features (i.e., arthritis or renal disease). People with only discoid lesions and no systemic features commonly have no auto-antibodies in their serum (i.e., antinuclear or anti-DNA tests will be negative). On the other hand, people with systemic lupus erythematosus are characterized by the presence of one or more types of auto-antibodies in their blood. From personal experience and from reviewing the literature, it has been estimated that between 5 and 10% of patients initially presenting with only the coin-shaped lesions of discoid lupus will, with time, develop systemic features. As noted above, approximately 20% of people with systemic lupus erythematosus will at the time of the initial presentation of their disease have discoid lupus lesions. These data indicate that, at times, the lupus disease process is dynamic and, with time, a small percentage of those patients who only have discoid lupus lesions will eventually develop systemic disease. In addition to these coin-shaped, scarring lesions, there are several different types of discoid lupus lesions with which patients should be familiar. Occasionally, the discoid lupus lesions may occur in the scalp producing a scarring, localized baldness termed alopecia. At times, these discoid lesions may appear over the central portion of the face and nose producing a characteristic butterfly rash. This type of lupus obviously has significant cosmetic implications. The discoid lupus lesions may develop thick, scaly (hyperkeratotic) formations and are termed hyperkeratotic or hypertrophic cutaneous lupus lesions. Discoid lupus lesions may also occur in the presence of thickening (deep induration) of the layers of underlying skin. This is termed lupus profundus. At the present time, research indicates that discoid lupus lesions are the result of an inflammatory process in the skin in which the patient's lymphocytes (predominantly T cells) play a major role. This is in contrast to systemic lupus erythematosus, where autoantibodies and immune complex formation are responsible for many of the clinical symptoms.
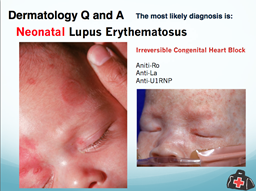
SUBACUTE CUTANEOUS LESIONS The second type of specific lupus lesion was most recently described by Sontheimer and Gilliam during the late 1970s. This lesion is characterized as a non-scarring, erythematosus (red), coin-shaped lesion which is very photosensitive (gets worse when exposed to UV light). This type of lesion, which is characteristic of subacute cutaneous lupus, occurs in lupus patients who, approximately 50% of the time, demonstrate features of systemic lupus erythematosus. Renal disease, however, is unusual in these patients. These skin lesions also occur in people who only have clinical evidence of skin disease, and do not show any symptoms of systemic lupus. Approximately 70% of people with these lesions have anti-Ro (SSA) antibodies. The subacute cutaneous lupus lesions can sometimes mimic the lesions of psoriasis or they can appear as non-scarring, coin-shaped lesions. These lesions can occur on the face in a butterfly distribution, or can cover large areas of the body. Unlike the discoid lupus lesions, these lesions do not produce permanent scarring, but can be of major cosmetic significance. Lesions of subacute cutaneous lupus may also be seen as a feature of neonatal lupus syndrome. Infants with neonatal lupus, born of mothers with anti-Ro (SSA) antibodies, may develop a transient lupus rash that disappears by the time they reach 6 months of age. At the present time, the best evidence suggests that the anti-Ro (SSA) antibody is passed via the placenta to the fetus and plays a major role in causing the characteristic lupus skin disease.
NON-SPECIFIC LUPUS LESIONS:
HAIR LOSS The non-specific lupus lesions include several forms of hair loss (alopecia) which are not related to the presence of discoid lupus lesions in the scalp. Systemic lupus patients who have been severely ill with their disease may (over a period of time) develop a transient hair loss in which large amounts of hair evolve into a resting phase and fall out. However, this is quickly replaced by new hair. In addition, a severe flare of systemic lupus erythematosus can result in defective hair growth which causes the hair to be fragile and to break easily. The hair is broken off above the surface of the scalp, especially at the edge of the scalp, giving the characteristic appearance termed "lupus hair."
VASCULITIS Systemic lupus erythematosus patients may develop inflammatory disease of the blood vessels (vasculitis). The cutaneous manifestations of vasculitis are varied. The lesions may appear as red welts involving large areas of the body. These lesions can also present as small red lines in the cuticle nail fold or on the tips of the fingers or as red bumps on the legs. In addition, these red bumps may ulcerate. At times, the blood vessels that are involved in this inflammatory process may be deep in the skin producing painful, red nodules. These are usually found on the legs.
PHOTOSENSITIVITY Photosensitivity is a common feature of lupus erythematosus. The overwhelming majority of specific lupus lesions (i.e., discoid lesions and subacute cutaneous lupus lesions) occur on sun-exposed areas. In addition, approximately 40-70% of people with lupus will note that their disease process, including the skin disease, is aggravated by sun exposure. Furthermore, people with subacute cutaneous lupus erythematosus, especially those who have anti-Ro (SSA) antibodies demonstrate pronounced photosensitivity. It has been estimated that 90% of patients with systemic or discoid lupus who have anti-Ro (SSA) antibodies are photosensitive. Furthermore, a number of these patients are so photosensitive that they will burn through window glass. Window glass filters out sunlight in the sunburn spectrum and protects normal people from developing a sunburn. However, window glass will not filter ultraviolet light of longer wavelengths and these wavelengths are capable of exacerbating (making worse) the skin lesions in people with lupus with anti-Ro (SSA) antibodies. One recent study has shown that ultraviolet light in both the sunburn and long wavelength light spectrum (those wavelengths that are not blocked by window glass) will cause lupus lesions to appear on the skin of patients with systemic lupus erythematosus, those with the lesions of subacute cutaneous lupus, and those who have only scarring lupus lesions (discoid lesions) with no evidence of systemic disease. These data provide excellent evidence for the role of ultraviolet light in the development of lupus skin lesions. There is clinical and experimental evidence that shows that ultraviolet light can also induce flares in people with systemic lupus erythematosus. The way that ultraviolet light triggers these systemic flares (or leads to the development of skin lesions) is not known. However, there is evidence that suggests that ultraviolet light is capable of leading to an increase in the number of auto-antigens to which the person is reacting.
TREATMENT The treatment of skin disease in lupus erythematosus involves the use of a number of drugs as well as the use of sunscreens. Individual lupus lesions can be treated with the topical application of steroid creams, the application of a steroid impregnated tape to cover the lupus lesion, or the intralesional injection of low doses of steroid. Widespread lupus lesions are frequently treated using hydroxychloroquine (Plaquenil) alone, or in combination with a short burst of oral steroids. On very unusual occasions, unmanageable, cosmetically objectionable lupus lesions have been successfully treated with vitamin A derivatives (such as Tegison). Sun protection can do a lot to prevent the development of lupus skin lesions. People with lupus should avoid prolonged periods of exposure to sunlight, especially between the hours of 10 am and 3 pm, when the sun is at its brightest. It is also a good idea to wear a wide-brimmed hat and avoid clothing made of thin fabric which will admit sunlight. In addition, the regular use of sunscreens with a sun protective factor rating of SPF 15 will also provide protection. In recent years, research has shown that ultraviolet light of long wavelengths, as well as ultraviolet light in the sunburn spectrum, is capable of producing lupus skin lesions. Sunscreens capable of blocking this long wave ultraviolet light are now available. In contrast to ordinary sunscreens which generally contain paraminobenzoic acid (PABA) esters and benzophones, these sunscreens are actually sunblocks and contain titanium oxide. For specific information regarding the treatment of various skin manifestations of lupus erythematosus, as well as the employment of sunscreens, consult your dermatologist, or your local chapter of the Lupus Foundation of America.
Depression In Lupus People with lupus often ask: "What degree of depression is normal?" and, "When should a patient seek professional help?" These questions reflect an awareness that depression occurs frequently in the course of lupus and that there is often an uncertainty as to whether or not it is to be expected because of the stresses and sacrifices imposed by the illness. The person with lupus is often aware that states of depression may be induced by the lupus, itself, by the various medications used to treat lupus, and by the countless factors and forces in a patient's life that are unrelated to lupus. What is meant by the term "depression?" The medical condition referred to as Clinical Depression is not to be confused with the transitory everyday experience of a mild mood swing that everyone experiences during difficulties. Just as we feel happy or fearful or jealous or angry, we are all "depressed" from time to time. On the other hand, Clinical Depressive Illness is a very disabling, unpleasant and prolonged state. By the way, it is the most common psychiatric condition seen in the general population (20% of women and 10% of men), as well as in medical practice. Clinical Depression may bring on a variety of physical and psychological symptoms: sadness and gloom, spells of crying (often without provocation), insomnia or restless sleep (or sleeping too much), loss of appetite (or eating too much), uneasiness or anxiety, irritability, feelings of guilt or remorse, lowered self-esteem, inability to concentrate, diminished memory and recall, indecisiveness, lack of interest in things formerly enjoyed, fatigue, and a variety of physical symptoms such as headache, palpitations, diminished sexual interest and/or performance, other body aches and pains, indigestion, constipation or diarrhea, etc. Not all people who suffer from Clinical Depression have all of the above symptoms. Patients are considered to be Clinically Depressed when they have a depressed mood, disturbances in sleep and appetite, and at least one or two of the symptoms mentioned above which last for several weeks and are severe enough to disrupt daily life. While there are many symptoms associated with Clinical Depression, there are seven which indicate the depth and degree of Depression. These are: sense of failure, loss of social interest, sense of punishment, suicidal thoughts, dissatisfaction, indecision, and crying. Two of the most common psychological signs of Clinical Depression are hopelessness and helplessness. People who feel hopeless believe that their distressing symptoms may never get better, whereas people who feel helpless think they are beyond help, that no one cares enough to help them or could succeed in helping, even if they tried. How Common is Depression in Those with Lupus? Some psychiatric and medical studies state that 15% of those with a chronic illness suffer from Clinical Depression; others place this figure as high as 60%. Although Clinical Depression is certainly more common in people with chronic medical illness, (e.g., SLE) than in the general population, not every patient with a chronic illness suffers from Clinical Depression. Episodes of Clinical Depression usually last for only a few months in patients with a chronic illness. Depressive Illness often goes unrecognized in those who have other medical illnesses because it presents symptoms so similar to those of the underlying medical condition. In systemic lupus erythematosus (SLE), symptoms of Depressive Illness such as lethargy, loss of energy and interest, insomnia, pain intensification, diminished sexual interest and/or performance, etc., can quite naturally be attributed to the lupus condition. Even in those individuals without chronic medical conditions, most cases of Depressive illness go unrecognized and untreated until the later stages of the illness when the severity of the Depression becomes unbearable to the patient, and/or until the family or physician can no longer ignore it. In fact, several studies indicate that between 3050% of cases of major Depressive Illness go undiagnosed in medical settings. Perhaps more disturbing is that many studies indicate that major depressive disorders in the medically ill are undertreated and/or inadequately treated, even when recognized. Many patients refuse to acknowledge that they are in a depressive state and will actually deny that they are feeling unhappy, demoralized or depressed. This group of individuals often experience what physicians called "masked" Depression. These patients resist the notion of emotional distress, substituting in its place various physical complaints. Physicians who are familiar with their patient's usual mood and personality, as well as their lifestyle and situation, are more likely to recognize changes associated with Depressive Illness. Similarly, patients are more apt to open up about their feelings when they are encouraged to do so by a physician they trust and with whom they are familiar. Unfortunately, there is all too common a distorted notion that those with a chronic illness have "reason to feel depressed because they are sick." This belief interferes with earlier recognition, earlier treatment, and earlier relief of suffering from Clinical Depression. This belief also ignores the fact that Clinical Depression in the physically ill generally responds well to standard psychiatric treatments and that patients treated only for their physical illness will suffer needlessly the effects of Clinical Depression. What is the Cause of Depression in Lupus? There is no one cause of Clinical Depression in lupus; rather, there are various and different factors contributing to Depression in chronic illnesses such as lupus. The most common cause is the emotional drain caused by the continuous series of stresses and strains associated with coping with the chronic illness and medical condition. Other causes may be the many sacrifices and losses required by the continuous life adjustments that a patient with a chronic illness must make. Various medications used to treat lupus, such as steroids (e.g., Prednisone), may induce Depression. Lupus involvement of certain organs (e.g., the brain, heart or kidneys) can also lead to Clinical Depression. There are also many unrecognized or unknown factors (which mayor may not be related to lupus) which may cause Depressive Illness. Of course, there are lupus patients who would develop Clinical Depression whether or not they had lupus. What is the Treatment and Prognosis for Depression in Lupus? Effective treatment requires early diagnosis and early intervention. Fortunately, most episodes of Depressive Illness in people with lupus are short-lived and subside on their own within a few months. Just as some lupus patients can tolerate a lot of pain, some seem to be able to accept and tolerate major symptoms of Depressive Illness without complaint. Depression is very stressful and anxiety producing, which may exacerbate the lupus. Depressive reactions should be treated with the same aggressiveness and persistence that one would use to treat a lupus flare, or any other medical complaint. Naturally, any underlying medical condition that could contribute to the Depression must be identified and controlled. Today, effective treatment is available for Depressive Illness and usually consists of psychotropic medication, psychotherapy and, most often, a combination of both. Anti-depressant medications are the drugs that are most often used; the four categories are;tricyclics, newergeneration nontricyclic anti-depressants, MAO inhibitors and lithium. The effectiveness of these medications may be increased by using them in combination or by the addition of other medications. Adequate and aggressive treatment involves the cooperation of the patient, and the support, education, and involvement of the patient's family and close friends. Such treatment may involve blood tests to determine the appropriate dosages of medication, open communication between the patient and treatment team, and a large ration of optimistic support in the form of encouragement, patience, availability and perseverance from the patient, his/her physician, and his/her family and close friends. Naturally, any underlying medical factors that contribute to the depressive state must be identified and addressed. Anti-depressant medications are associated with various side effects and may intensify various symptoms associated with lupus (e.g., increase in the drying of mucous membranes in Sjogren's Syndrome). When anti-depressant medications are effective, there is a welcome improvement in the patient's sense of wellbeing and overall attitude and adjustment. Recovery from Depression is usually a gradual process. Dramatic improvements do not usually occur in a few days; however, one begins to see some progress after a few weeks. Even when signs of Clinical Depression seem to clear quickly, it is not unusual for an individual to relapse when the medication is stopped. For this reason, medication should be continued for approximately six months or longer and the dosage should be tapered slowly over a 3-4 week period when treatment is discontinued. In patients with Depressive Illness, there is often a general slowing and clouding of mental functions (cognition). These troublesome and not infrequent disruptions in mental functioning tend to go under reported to their physicians and are rarely confirmed to be due to any specific structural change. Fortunately, these transient alterations in mental functioning improve as the depressive condition improves. Psychotherapy can be very helpful in assisting people with Clinical Depression to work through and understand their feelings, their illness and their relationships, and to cope more effectively with stress and their life situation. The benefits to the patient are best served when the primary care physician maintains a close relationship with their psychiatrist or psychologist. Such a working relationship maximizes the quality of patient care and provides the most powerful approach to the management of depression.
Antiphospholipid Antibodies And Systemic Lupus Erythematosus What are antiphospholipid antibodies? There are several kinds of antiphospholipid antibodies. The most widely measured are the lupus anticoagulant and anticardiolipin antibody. These antibodies react with phospholipid, a type of fat molecule that is part of the normal cell membrane. Lupus anticoagulant andanticardiolipin antibody are closely related, but are not the same antibody. This means that someone can have one and not the other. There are other antiphospholipid antibodies, but they are not commonly measured. How common are antiphospholipid antibodies? As with other autoantibodies (antibodies directed against one's self) in lupus, the antiphospholipid antibodies can come and go in any individual patient. It turns out that there are many ways to measure these antibodies, and different methods may not always give the same result. For example, in different studies, 8 to 65 percent of people with lupus have the lupus anticoagulant, and 25 to 61 percent have anticardiolipin antibody. These antibodies can also be found in people who do not have lupus. For example, two percent of young women have anticardiolipin antibody. These antibodies were first discovered in people who have lupus, but it is not necessary to have lupus to have these antibodies. In fact, in most studies, over 50% of people with these antibodies do not have lupus. We do not understand why a person's immune system begins to manufacture these antibodies. Why are antiphospholipid antibodies important? The presence of both the lupus anticoagulant and anticardiolipin antibody is increased in lupus patients who have had thrombotic (bloodclotting) complications such as deep venous thrombosis("thrombophlebitis"), stroke, gangrene, and heart attack. Studies suggest that the presence of these antibodies may also increase the future risk of thrombotic events. Anticardiolipin antibody has been found to be increased in pregnant women with lupus who have had miscarriages. The combination of thrombotic problems, miscarriages, and a low platelet count has been called the "Antiphospholipid Antibody Syndrome." It is not necessary to have lupus to have the Antiphospholipid Antibody Syndrome. It is important for doctors to realize this and to check people who have had a stroke, heart attack, or miscarriage for no known reason to see if they have these antibodies. Antiphospholipid antibodies interfere with the normal function of blood vessels, both by causing narrowing and irregularity of the vessel(called "vasculopathy"), and by causing clots in the vessel (called "thrombosis"). These blood vessel problems can then lead to complications such as stroke, heart attack, and miscarriage. How do doctors test for antiphospholipid antibodies? Blood tests are used to identify antiphospholipid antibodies. Specialized tests which measure blood clotting (coagulation tests) are used to find the lupus anticoagulant. The activated partial thromboplastin time (aPTT) is a widely available blood clotting test that is often used. If the aPTT is normal, more sensitive coagulation tests should be done to test for the lupus anticoagulant. These more sensitive tests include the modified Russell viper venom time (RVVT),the platelet neutralization procedure (PNP), and the kaolin clotting time (KCT). If the clotting test is prolonged (the number of seconds that it takes the blood to clot is longer), the physician will suspect that the lupus anticoagulant is present. This is confusing, because even though the blood takes longer to clot in the test tube, the blood actually clots more easily in the person's body. The anticardiolipin antibody is measured in an ELISA test. There are many classes of anticardiolipin antibody (IgG, IgM, IgA). It is possible to test for all of these antibody classes at once or the physician may wish to test for each one separately. The IgG type of anticardiolipin antibody is the type that is most often associated with complications. Sometimes, there are technical difficulties with the IgM test, making it more difficult to interpret the results of this test. Some lupus patients with very high IgM anticardiolipin antibody have a problem called hemolytic anemia, in which their immune system attacks their red blood cells. Since antiphospholipid antibodies can come and go, how often should doctors check for them in lupus patients? There are no current recommendations on the timing of repeat tests. Certainly the antiphospholipid antibodies should be checked in people who have had thrombotic problems, miscarriages, or low platelet counts. What is the treatment for a person who has antiphospholipid antibodies? If a person has the lupus anticoagulant or anticardiolipin antibody, but has never had a thrombotic complication, treatment is not currently recommended. If a patient has had a thrombotic complication and has these antibodies, treatment may depend on where the clot (thrombosis)occurred. In general, treatment consists of "thinning" the blood to prevent future clots, using either aspirin or warfarin (Coumadin). How successful is treatment in people who have had a thrombosis (clot) in association with these antibodies? Some individuals who had initially been treated with aspirin have had a second episode of thrombosis and have then been treated with warfarin(Coumadin). A few of these patients had a second episode of thrombosis while on warfarin. However, treatment with warfarin appears to be successful overall. The length of time that this treatment is necessary is unclear. Many physicians recommend long-term or even life-long treatment to prevent future episodes of thrombosis. If a woman has antiphospholipid antibodies and is pregnant, how is it treated? If the woman has antiphospholipid antibodies and is pregnant for the first time, or has had normal pregnancies in the past, no treatment maybe advised. However, if the woman has had miscarriages in the past, several different treatment regimens are available, including aspirin, Prednisone, and/or subcutaneous shots of a blood thinner called Heparin. Pregnancies in women with antiphospholipid antibodies are considered to be "high risk pregnancies." It is necessary for the obstetrician or gynecologist to work closely with the rheumatologist or other physician who evaluates a woman with miscarriages for antiphospholipid antibodies. Miscarriages, especially early in pregnancy, are not rare. Women who have had multiple miscarriages should be checked to see if they have Medications Used In The Treatment Of Lupus Medications are a very important aspect of the management of many patients with systemic lupus erythematosus (SLE). There are two basic goals of drug treatment: 1) to reduce the inflammation within the affected tissues, and 2) to suppress abnormalities of the immune system that are considered to be responsible for the tissue inflammation. This pamphlet discusses the principal drugs used in the primary management of lupus. In addition, it is important to note that people with lupus often require other drugs for the treatment of complications commonly seen with the disease. Examples of these types of medications include diuretics for fluid retention, anti-hypertensive drugs for increased blood pressure, anti-convulsants for seizure disorders, and antibiotics for the treatment of infections. Anti-Inflammatory Drugs Anti-inflammatory drugs relieve the symptoms of lupus by reducing the inflammation responsible for the pain and discomfort of the disease. By far, anti-inflammatory medications are the most commonly prescribed drugs for lupus treatment, particularly for symptoms such as low-grade fever, fatigue, arthritis, or pleurisy. Improvement in symptoms is generally noted within several days of beginning treatment. In the majority of people with lupus, anti-inflammatory drugs are all that is ever required to control their lupus. Anti-inflammatory drugs fall into two categories: non-steroidal agents or corticosteroids. Among drugs of the non-steroidal class, salicylates(usually in the form of aspirin) are most commonly used. The aspirin is often enteric-coated or buffered with an antacid to reduce gastrointestinal symptoms. As an alternative to salicylates, a number of other non-steroidal drugs are available. Some of these drugs require a physician's prescription and others, such as ibuprofen, may be directly purchased without a prescription. For reasons that aren't known, people often respond better to one non-steroidal drug than another. Thus, it may be necessary to give brief courses of several different drugs to determine the most effective one. The most common side effect associated with non-steroidal medications is irritation of the stomach or bowel causing abdominal pain. Infrequently, this may lead to serious complications such as an ulcer with bleeding. To reduce the chance of these problems, non-steroidal drugs are usually taken with meals or given along with other medications that protect the stomach and bowel. Several very rare side effects of non-steroidal drugs may be mistaken for signs of lupus. The drugs may cause fever or skin rashes that can easily be confused with signs of active lupus. The drugs may produce changes in the kidney leading to edema or abnormalities on urinalysis or blood tests that resemble lupus nephritis. Similarly, non-steroidal drugs have been shown to cause fever and headache that can mimic a type of neurologic disease seen in lupus. Recognition of these side effects is important since the symptoms are promptly reversed simply by stopping the drug. Corticosteroids (Cortisone)Corticosteroids are drugs with very potent anti-inflammatory properties. They may be used as creams or ointments for lupus skin rashes or given as pills or injections. Most signs of lupus respond rapidly to corticosteroid treatment and at times, corticosteroids may actually be life saving. The decision to begin corticosteroids and the details as to what type and dose of corticosteroid to use is highly individualized and depends on the needs of the patient. Patients with symptoms such as fever, arthritis, or pleurisy that have not responded to non-steroidal drugs are generally treated with low doses of an oral corticosteroid such as Prednisone or methylprednisolone (Prednisolone). On the other hand, patients with more severe or serious manifestations of lupus, such as nephritis with massive proteinuria, anemia or low platelets(thrombocytopenia), or seizures may require high doses of corticosteroids. In most instances, the corticosteroid is given as a single dose in the morning. Other ways of giving corticosteroids include doses given several times each day, doses only on alternate days, or in high doses by intravenous infusion (bolus therapy). In general, once the symptoms of lupus have responded to treatment with corticosteroids, the dose is gradually reduced (tapered) while the patient is carefully watched for evidence of relapse of the disease. The longer a person has been on corticosteroids, the more difficult it becomes to lower the dose. There are many complications of corticosteroid treatment. In general, the risks of these complications are increased when high doses of corticosteroids are required or when corticosteroids are used for an extended period. Corticosteroids may produce changes in physical appearance such as weight gain, puffiness of the cheeks, thinning of the skin and hair, and easy bruising. Stomach discomfort such as dyspepsia or heartburn are common and may be minimized by giving the drug with meals or along with medications that prevent stomach damage. Patients may note marked changes in mood while taking corticosteroids including both depression and emotional lability (mood swings). Corticosteroids may cause diabetes, increase the risk of infections, or when given for many months may cause cataracts. Corticosteroids may have an effect on the bones, producing joint damage of the hips, knees, or other joints (osteonecrosis).Corticosteroids may also produce osteoporosis (thinning of bone) when given over long periods. For many, calcium or other medications to prevent osteoporosis is given along with the corticosteroids. Anti-Malarial Drugs- Drugs used for the treatment of malaria (anti-malarial drugs) are widely used in the management of lupus symptoms. Anti-malarials are particularly effective in the treatment of lupus arthritis, skin rashes, and mouth ulcers. The drug hydroxychloroquine (Plaquenil) is the most commonly used of the anti-malarial agents. Anti-malarials are considered to have a small risk of harming a fetus and are often discontinued in the lupus patient who becomes pregnant. The side effects of low-dose anti-malarial therapy include gastric symptoms (stomach pain or dyspepsia), rashes or darkening of the skin, and muscle weakness. Shortly after starting treatment, there may be a mild blurring of vision that entirely clears on its own. In high doses such as those used in the treatment of malaria, anti-malarial drugs may damage the retina of the eye to produce visual disturbances, including blindness. The risk of this complication with the low doses of anti-malarials used in the treatment of lupus is extremely low. However, as a precaution, patients treated with anti-malarials generally have a thorough eye examination before treatment with the drug is initiated and then every 6 months during LUPUS and the Liver Involvement of the liver in SLE is a frequently misunderstood complication of the disease. The liver can be affected as a result of lupus itself, as well as the medications used to treat inflammation caused by lupus. There is also a specific inflammatory disease of the liver, related to SLE, called lupoid hepatitis. This column attempts to reconcile our perceptions of what "lupus in the liver" really means. Lupus can affect the liver in numerous ways that are delineated below:
ENLARGEMENT OF THE LIVER, or hepatomegaly, is found in 10% of SLE patients. The liver is rarely tender unless the enlargement is so great that the capsule (or covering) of the organ is stretched. The most common cause of large livers in lupus include lupoid hepatitis, congestive heart failure, or cirrhosis.
JAUNDICE, in which the person's skin has a yellowish hue, is seen in 1-4% of patients with SLE. Manifested by high levels of bilirubin which are responsible for this pigmentation, jaundice results from autoimmune hemolytic anemia, viral hepatitis, cirrhosis, or bile duct obstruction (from gallstones, tumor, or pancreatitis). Occasionally, certain medications including nonsteroidal anti- inflammatory drugs and azathioprine may produce jaundice.
HEPATIC VASCULITIS, or inflammation of the small and medium sized arteries of the liver, is extremely rare and is noted in one lupus patient per thousand. It responds to corticosteroids.
BUDD-CHIARI SYNDROME (which is very rare) results from a blood clot in the portal veins which drain materials from the liver. Lupus patients with the lupus anticoagulant, anticardiolipin antibody, or antiphospholipid syndrome appear to be uniquely at risk for developing these clots. Additionally, hepatic artery clots may occur. Untreated Budd-Chiari can lead to ascites, portal hypertension, and liver failure. The preferred treatment of Budd-Chiari syndrome is anticoagulation (blood thinning).
ASCITES is a term which refers to fluid in the abdomen as a result of the manufacture of this liquid by the peritoneum, or lining of the abdominal cavity. Often associated with serositis (or similar fluid being made by the pleura or pericardium which line the lung and heart), ascites causes swelling of the abdomen and is noted in 10% of patients with SLE. Usually reflecting active disease, it may be painless or painful and can be mistaken for a "surgical abdomen" resulting in unnecessary surgery. If an infection is ruled out, ascites is treated with anti inflammatory medication, gentle diuresis, and occasionally periodic drainage. Ascites also may result from liver failure or nephrotic syndrome.
ABNORMAL LIVER FUNCTION TESTS may be found in 30-60% of patients with SLE. Blood enzyme evaluations included in routine blood panels such as the AST (also called SGPT), ALT (also called SGOT), alkaline phosphates and GGT may be slightly elevated as a result of a variety of mechanisms. First of all, nearly all nonsteroidal antiinflammatory agents, as well as aspirin, can elevate these enzymes, and lupus patients appear to be particularly susceptible to this. These minor abnormalities are usually of little consequence and I ignore them unless they are greater than three times normal. Also, active lupus can elevate these enzymes. Most nonsteroidals can be stopped for a week or two and the enzymes rechecked. If they remain increased, the possibilities for this elevation include hepatitis, infection, biliary disease, alcoholism, or active lupus. This leaves us with the most perplexing problem to discuss: lupoid hepatitis. Described by Joske and King in 1955 and named by Mackay in1956, lupoid hepatitis has undergone many changes in definitions. The overwhelming majority of patients who were told they had lupoid hepatitis between 1955 and 1975 would not fulfill current criteria for this disease. Initially thought of as the presence of chronic active hepatitis (hepatitis means inflammation of the liver) with LE cells, the term "autoimmune hepatitis" seemed more appropriate since few of these patients had typical clinical lupus. The development of diagnostic tests to detect hepatitis A, B, and more recently C changed our concepts of lupoid hepatitis. The current working definition of lupoid hepatitis is: 1. liver pathology consistent with chronic active hepatitis 2. absence of evidence for active hepatitis virus A, B or C infection 3.a positive ANA or LE cell prep Even using these criteria, only 10% of patients at the Mayo Clinic fulfilled the American College of Rheumatology (ACR) criteria for SLE. Although fevers, joint aches, malaise and loss of appetite are common(as well as jaundice with itching), many of the physical findings we associate with SLE (rashes, other organ involvement) are usually absent. This is further complicated by the knowledge that lupus patients have compromised immune systems and can develop a viral hepatitis, take liver-toxic medications, and some abuse alcohol just as non-lupus patients do, which can lead to chronic active hepatitis.
Fibromyalgia What is Fibromyalgia? Fibromyalgia syndrome is a common form of generalized muscular pain and fatigue. The name "fibromyalgia" means pain in the muscles and the fibrous connective tissues (the ligaments and tendons). This condition is referred to as a "syndrome" because it's a set of signs and symptoms that occur together. (A sign is what the physician finds on examination;a symptom is what a person reports to the doctor.) Fibromyalgia is especially confusing and often misunderstood because almost all it symptoms are also common in other conditions. In addition, it does not have a known cause. The name "fibromyalgia" has largely replaced the term "fibrositis," which was once used to describe this disorder. The "it is" means "inflammation" - a body process that can result in pain, swelling, warmth, redness, and stiffness. Early reports of this condition described inflammation in muscles. However, during the past 50 years investigators have proven that inflammation is not a significant part of fibromyalgia. Fibromyalgia is a form of "soft-tissue" or muscular rheumatism rather than "arthritis of a joint." The word "rheumatism" refers to pain and stiffness associated with arthritis and related disorders of the joints, muscles, and bones. Fibromyalgia mainly affects muscles and their attachments to bones. Therefore, although fibromyalgia may feel like a joint disease, it is not a true form of arthritis and does not cause deformities of the joints. Unfortunately, because certain syndromes lack physical and laboratory findings (signs), but depend mostly on a person's report of complaints and feelings (symptoms), these syndromes are often viewed as not being real or important. In the past, fibromyalgia suffered from this type of negative thinking. Over the past ten years, however, fibromyalgia has been better defined through studies that have established guides for its diagnosis. These studies have shown that certain complaints, such as generalized muscular pain and tender points, are present in people with fibromyalgia and not commonly present in healthy people or people with other rheumatic conditions. These diagnostic features separate fibromyalgia from other types of conditions that have chronic muscle and bone pain.
Symptoms and Signs Pain- Pain is the most prominent symptom of fibromyalgia. It is generally felt all over, although it may start in one region, such as the neck and shoulders, and seems to spread over a period of time. Fibromyalgia pain has been described in a variety of ways including: burning, radiating, gnawing, sore, stiff, and aching. It often varies according to time of the day, activity level, weather, sleep patterns, and stress. Most people with fibromyalgia say that some degree of pain is always present. They sense that the pain is mainly in their muscles and often note that fibromyalgia feels like a persistent flu. For some people with fibromyalgia the pain may be quite severe. Although the general physical examination is usually normal, and individuals may look well, careful examination of their muscles will demonstrate very tender areas at specific locations. The presence and pattern of theses characteristic "tender points" separate fibromyalgia from other conditions. Not all physicians are familiar with the evaluation of these tender points. However, most rheumatologists (specialists in arthritis and rheumatism) do know when and how to perform such an examination. The tender areas in fibromyalgia are similar in location to sore and tender areas in other common muscle and bone pain disorders such as tennis elbow and trochanteric bursitis (inflammation of the outer side of the hip). They are found in many locations and are almost always on both sides of the body. People often are not aware of the exact location or even the presence of many of these tender points until they are specifically examined by a doctor. Fatigue and Sleep Disturbances About 90 percent of people with fibromyalgia describe moderate or severe fatigue with lack of energy, decreased exercise endurance, or the kind of exhaustion felt with the flu or with lack of sleep. Often the fatigue is more of a problem and more troubling than the pain. Generally, people with fibromyalgia wake up feeling tired, even after sleeping throughout the night. They may be aware that their sleep has become lighter and that they wake up during the night. Scientific studies have demonstrated that most people with fibromyalgia have an abnormal sleep pattern, especially an interruption in their deep sleep. The fatigue in fibromyalgia is similar to the in another condition called chronic fatigue syndrome (CFS). Some people with fibromyalgia have symptoms of CFS, and vice versa. for example, many people with CFS have the tender points and symptoms considered to be diagnostic of fibromyalgia. Because there is an overlap in these two common syndromes, it may not be possible to separate these two conditions, and one doctor may give a diagnosis of fibromyalgia whereas another may call the condition chronic fatigue syndrome. Nervous Systems Symptoms Changes in mood and thinking are common in fibromyalgia. Many individuals feel "blue" or "down," although only about 25 percent are truly depressed. Some people also feel very anxious. Generally, the depression and anxiety seem to follow the onset of fibromyalgia symptoms and may be the result of the fibromyalgia rather than a cause of it. However, some researchers feel there may be a "biologic link" between fibromyalgia and some forms of depression and chronic anxiety. As with other chronic illnesses, people with fibromyalgia may report difficulty concentrating or performing simple mental tasks. There is no evidence that these problems become more serious. Similar problems have been noted in many people with sleep disturbances of all kinds or with mood changes. People with fibromyalgia may have feeling of numbness and tingling in their hands, arms, feet, legs, or sometimes in their face. These feeling can suggest other disorders such as carpal tunnel syndrome, neuritis, or even multiple sclerosis. Therefore, people with fibromyalgia often undergo numerous tests for such conditions, only to find that the test results are normal. Other Problems Headaches, especially muscular (tension) and migraine headaches, are common in fibromyalgia. Abdominal pain, bloating, and alternating constipation and diarrhea are also common. This may resemble irritable bowel syndrome or "spastic colon." Similar bladder spasms and irritability may cause urinary urgency or frequency. The skin and circulation are often sensitive to temperature and moisture changes, resulting in temporary changes in skin color. How is Fibromyalgia Diagnosed? Fibromyalgia is diagnosed by the presence of widespread pain in combination with tenderness at most of the specific locations. Unfortunately, no one laboratory test or x-ray can diagnose fibromyalgia. Such tests are only helpful when they prove the presence of other conditions, such as low thyroid hormone, (hypothyroidism),which can cause fibromyalgia signs and symptoms. A careful history and physical examination can identify other conditions that may cause chronic pain and fatigue and identify the "tender point" that are seen in fibromyalgia. Because the complaints of fibromyalgia are so general and often bring to mind other medical disorders, many people undergo complicated and often repeated evaluations before they are diagnosed as having fibromyalgia. Furthermore, since not all doctors have been trained to recognize this disorder, it is important for people to see a rheumatologist or other doctor who is very familiar with the diagnosis and treatment of this condition. What Causes or Triggers Fibromyalgia? The single exact cause of fibromyalgia is unknown. Many different factors, alone or in combination, may trigger this disorder. For example, a number of stresses - such as an illness, physical trauma, emotional trauma, or hormonal changes - may precipitate the generalized pain, fatigue, sleep, and mood problems that characterize fibromyalgia. Physical or emotional trauma could precipitate fibromyalgia in a number of ways. For example, a physical trauma such as having an infection or flu could lead to certain hormonal or chemical changes that promote pain and worsen sleep. In addition, people with fibromyalgia may become inactive, depressed, and anxious about their health, further aggravating the disorder. In recent years, studies have shown that in fibromyalgia the muscle is especially vulnerable to decreased circulation and minor injury. Therefore, smoking and inappropriate exercise or poor posture may aggravate fibromyalgia. Research has also looked at the role of certain hormones or body chemicals that may alter pain, sleep, and mood. Eventually, this research should result in a better understanding of fibromyalgia, as well as more effective treatment, and even prevention! How is Fibromyalgia Treated? Currently, treatment o fibromyalgia includes: medications that diminish pain and improve sleep exercise programs that involve muscle stretching and improve cardiovascular fitness relaxation techniques and other measures to help you relax tens muscles educational programs to help you cope with fibromyalgia. As with most chronic illnesses, the treatment should be tailored to meet your individual needs. Some people with fibromyalgia have mild symptoms and need very little treatment once they understand what fibromyalgia is and what worsens their condition. Most people do benefit from a comprehensive care program.
Medications The anti-inflammatory medications used to treat arthritis and many rheumatic conditions do not have a major effect in fibromyalgia. However, modest doses of aspirin, ibuprofen, or acetaminophen may help to provide some pain relief and lessen stiffness. Narcotic pain relievers, tranquilizers, and cortisone derivatives have been shown to be ineffective and should be avoided because of their potential side effects. Medications that promote deeper sleep and also relax muscles help many people with fibromyalgia. These include amitriptyline (Elavil), doxepin (Sinequan), cyclobenzaprine (Flexeril), and related medications. Although these medications are also used to treat depression, in people with fibromyalgia they are generally used in very low doses and only at bedtime. Thus, they are not specifically used as antidepressants or tranquilizers in the treatment of fibromyalgia but may relieve pain and improve sleep. Although many people sleep better and have less discomfort when they take these medications, the improvement varies greatly from person to person. In addition, the medications may have side effects such as daytime drowsiness, constipation, dry mouth, and increased appetite. These side effects are rarely severe, but can be disturbing and may limit the use of these drugs. Therefore, a number of different medicines may need to be tried and doses adjusted in consultation with a doctor.
Exercise and Physical Therapy Two principles of treating fibromyalgia are to increase cardiovascular (aerobic) fitness and to stretch and mobilize tight, sore muscles. You may be reluctant to exercise if you are already in pain and feel tired. Low or non-impact aerobic exercises such as brisk walking, biking, swimming, or water aerobics are generally the best way to start such a program. Exercise on a regular basis, such as every other day, and gradually increase to reach a better level of fitness. Gently stretch your muscles and move your joints through an adequate range of motion daily and before and after aerobic exercise. Physical therapy may be helpful and could include techniques such as: heat, ice, massage, whirlpool, ultrasound, and electrical stimulation to help control pain. Physical therapists may also be consulted to design a specific exercise program to improve posture, flexibility, and fitness. Coping with Fibromyalgia Often people with fibromyalgia have undergone many tests and have seen many different specialists while in search of an answer. This leads to fear and frustration, which may increase the pain. People with fibromyalgia are often told that since they look well and their tests are normal, they are not suffering from a real disorder. Their family and friends, as well as physicians, may doubt the reality of their complaints, increasing their feelings of isolation, guilt, and anger. You and your family should understand that fibromyalgia is a real cause of chronic pain and fatigue and must be dealt with as with any chronic illness. Yet, fibromyalgia is not life-threatening and causes no deformity. Although symptoms may very, the overall condition rarely worsens over time. Often just knowing fibromyalgia is not a progressive, crippling disease allows people to stop additional expensive testing and to develop amore positive attitude toward their condition. Relaxation techniques, such as meditation, visual imagery, progressive muscle relaxation, yoga, or biofeedback may also be helpful. You should examine your own sleep patterns and avoid aggravating factors such as excess caffeine and alcohol. If you feel depressed or very anxious, it is important to get help from a mental health professional. The more you learn about your condition, and the more you take an active role in finding the best means to lessen your symptoms, the better the outcome. Support groups and educational classes organized by the Arthritis Foundation have been a source of help for many people with fibromyalgia. Just knowing that you are not alone can be a source of support. Some people with fibromyalgia have such severe symptoms that they are unable to function well at work or socially. These individuals may require greater attention in a program that employs physical or occupational therapists, medical social workers, rheumatology nurses, mental health professionals, rehabilitation counselors, and sleep specialists. In summary, fibromyalgia is a common cause of chronic, generalized pain. It is not damaging to the body in any way, but it is usually a painful disorder that does not go away and waxes and wanes. For example, levels of pain and fatigue in some people appear to be as bad as in rheumatoid arthritis. Since fibromyalgia may interfere with all aspects of a person's life, a carefully planned treatment program is essential. This begins with a correct diagnosis and a detailed explanation of the condition.
Cardiopulmonary Disease And Lupus The heart and the lungs are frequently affected in patients with Systemic Lupus Erythematosus (SLE). The degree of cardiopulmonary involvement ranges from no symptoms to life-threatening complications. In fact, heart disease is the third most common cause of death in people with SLE.
CARDIAC (HEART) INVOLVEMENT. Lupus can involve all parts of the heart including; the pericardium (sac surrounding the heart), myocardium (muscle layer), endocardium (lining of the inside of the heart) and the coronary arteries. Pericarditis (inflammation of the sac around the heart) is the most common disease involving the heart in people with lupus. It occurs when the lining of the pericardium is attacked by autoantibodies and becomes inflamed. The usual symptoms include sharp chest pain underneath the sternum, fever, rapid heart beat and occasionally, shortness of breath. The pain can change with changes in position. Frequently, it is relieved by leaning forward slightly. The chest pain may feel like the pain associated with a heart attack. In some cases of pericarditis patients may have no symptoms. Blood tests, chest X-rays, an EKG, and an echocardiogram may be ordered to help diagnose pericarditis. The echocardiogram is an ultrasound of the heart and will tell the physician if there is fluid around the heart. In people with lupus, it is not uncommon to find an excess amount of fluid around the heart. Because pericarditis can be caused by conditions other than lupus, the cause must be determined before treatment begins. If pericarditis is caused by infection or kidney failure, the treatment is different than if it is due to lupus. Lupus pericarditis can be treated with anti-inflammatory agents. If this form of therapy is unsuccessful, a brief course of corticosteroid treatment is usually needed. When lupus causes inflammation of the myocardium, myocarditis occurs. Significant heart muscle disease is not common in SLE. The symptoms of myocarditis include: an unexplained rapid heart beat, anabnormal electrocardiogram, an irregular heart beat and heart failure. Myocarditis is frequently associated with inflammation of other muscles in the body. Treatment of lupus myocarditis usually includes corticosteroids. Immunosuppressive drugs (Cytoxan, Imuran) may be added if the inflammation is not completely controlled with steroids. Myocarditis can lead to tissue damage and replace heart tissue with scar tissue. When lupus causes inflammation of the endocardium (endocarditis), the heart valves can be damaged, but it rarely effects the pumping.
Joint And Muscle Pain In Lupus Joint and muscle pains are very common symptoms of systemic lupus erythematosus (SLE). In fact, ninety percent of people with lupus will experience joint and/or muscle pain at some time during the course of their illness. The problems of patients with the joint and muscle inflammation of SLE are varied. Frequently, the aching pain in joints(arthralgia) and muscles (myalgia) may mimic a viral or flulike illness. Others may have the characteristic symptoms of arthritis, that is, joints that are not only painful but also swollen, warm and tender. Still others with intense muscle inflammation (myositis) may have progressive weakness and loss of strength in addition to muscle pain. Joint and/or muscle pain can occur at any time during the course of SLE, or may even precede the other symptoms of the disease by months or years. However, it must be emphasized that although muscle and joint pains are common symptoms of lupus, SLE is an infrequent cause of these symptoms. For example, joint pain is more commonly caused by osteoarthritis or rheumatoid arthritis than by SLE. Therefore, a diagnosis of SLE must be based on a thorough physical examination, a detailed medical history and the results of specialized laboratory tests in addition to symptoms of muscle and joint pain.
Lupus Arthritis The joint pain of lupus arthritis often comes and goes. Individual attacks may last several days or weeks and then subside, only to recur at a later date. The joints farthest from the trunk of the body (i.e., fingers, wrists, elbows, knees, ankles) are most frequently involved, usually several at a time. Stiffness and pain in the morning, which improves as the day goes on, is characteristic of lupus arthritis. Later in the day, as the individual becomes more tired, the aches may return. Another characteristic of lupus arthritis is that the pain is usually symmetrical, which means that it affects similar joints on both sides of the body. Therefore, a single, chronically painful and swollen joint, even in a person who has been diagnosed with lupus, is most likely due to some other cause. Backaches or neck pains are not caused by lupus arthritis since the spine is not involved in lupus. Unlike osteoarthritis, lupus arthritis does not usually cause deformities or destruction of the joints. This lack of damage to the joints is observed both clinically and by xray, even after months of joint symptoms. Diagnosis. The pattern of joint pain and the setting in which it occurs are the best clues in determining if the pain is caused by SLE or not. X-rays of the painful joints are usually normal in people with lupus arthritis. An examination of the synovial fluid within a swollen joint may be performed to determine if there is a low grade inflammatory reaction. However, these studies are used to rule out other possible causes for the joint pain, and not to establish a diagnosis of SLE. In fact, when arthritis is the only symptom of lupus, diagnosis can be very difficult, if not impossible. In these cases, careful observation and reevaluation by a physician as other symptoms of SLE evolve is essential in making a diagnosis of lupus. Laboratory tests such as the anti-nuclear antibody (ANA) test and the test for rheumatoid factor can sometimes be helpful. At least 67 percent of persons with rheumatoid arthritis will have an antibody(rheumatoid factor) in their blood. At least 95 percent of persons with SLE will have various forms of another antibody (anti-nuclear antibody)in their blood. However, it must be emphasized that neither of these antibodies is specific for rheumatoid arthritis or SLE. Each occurs in about 25 percent of patients with either disease, and in a large number of other conditions. Treatment. One of the most common misconceptions about arthritis is that there is no satisfactory treatment currently available. On the contrary, proper and early treatment for most forms of arthritis does exist, and can significantly retard joint damage and lessen the pain of arthritis. Lupus arthritis is usually treated with non-steroidal, anti-inflammatory medications (e.g., aspirin, ibuprofen, naproxen).These medications are effective in the majority of cases and are usually well tolerated. However, when this line of therapy is not effective, anti malarial drugs such as hydroxychloroquine (Plaquenil)may be added. Corticosteroids (Prednisone) are used rarely and only when the joints remain swollen and painful despite other treatment. Cytotoxic medications should not be used to treat only lupus arthritis. It is also important that a person learn joint protection procedures to be able to rest his or her joints during flares of lupus arthritis. Lupus Myositis Unlike the joints, the muscles can be seriously damaged by SLE. This damage may result in muscle weakness and loss of strength unless early, appropriate treatment is given. Inflamed muscles may not only be painful, but may also be tender to the touch. Muscle weakness is the most common symptom of lupus myositis. Characteristically, the muscles of the trunk of the body are affected(i.e., neck, pelvic girdle and thighs, shoulder girdle and upper arms).Pain in the small muscles of the hand or weakness of the grip are not symptoms of SLE myositis. However, nerves as well as muscle fibers can be caught up in the inflammatory process and, occasionally, weakness of the wrists and hands or the ankles and feet may occur as a result of nerve damage. Diagnosis. The diagnosis of SLE myositis is relatively straightforward. There are chemical enzymes (e.g., CPK, SGOT, SGPT, aldolase) which are normally concentrated within muscle fibers and which escape into the blood circulation when muscle fibers are being damaged by inflammation. Thus, tests for these chemicals in the blood are abnormal in SLE myositis. These tests can also be used to determine the severity of muscle involvement: more severe myositis results in a higher level of these enzymes in the blood. Such tests are therefore useful in the diagnosis of SLE myositis, and in following the course of the disease and its response to therapy. Just as the electrocardiogram (EKG) reflects damage to heart muscle, the electromyogram (EMG) can be used to determine the character of muscle damage in lupus myositis. When inflammation is present, the EMG shows a characteristic pattern of electrical response. A microscopic examination of a sample of muscle tissue a biopsy) may also be taken from a painful muscle to confirm the presence of inflammation and to help identify the severity of the inflammation. Treatment. Corticosteroids (Prednisone) are necessarily prescribed for the treatment of SLE myositis. High doses (50 mg. per day or more of Prednisone or equivalent) are initially given for prompt suppression and control of the inflammation. The steroid dose is gradually reduced as the inflammation subsides, as determined by the patient's symptoms and enzyme levels in the blood. The vast majority of people with lupus respond promptly and well to corticosteroids. It is seldom necessary to augment treatment with cytotoxic or immunosuppressive medications. Once the acute, inflammatory phase is past, a well directed exercise program should be started to help the patient regain normal muscle strength and function.
Musculoskeletal Complications of SLE and Its Therapy Corticosteroids, either taken alone or in combination with cytotoxic agents, are used to control certain manifestations of lupus (e.g., major organ involvement, myositis, severe blood abnormalities). Such therapy, when required in high and sustained doses, can sometimes result in bone damage and muscle weakness. However, such complications are seldom due to the effects of the medications alone, but are often due to a combination of factors. For example, lupus patients may be more susceptible to infections, including joint infections, because of the use of corticosteroids and immunosuppressive medications. People with SLE who have been taking steroids for prolonged periods of time can develop ischemic necrosis of bone (also called aseptic necrosis or avascular necrosis). This condition is caused by altered blood flow to a portion of bone which results in the death of that area of bone. As the body repairs this area of dead bone, a weakening of the bone occurs and a portion of the bone surface may collapse. The hips, shoulders and knees are the areas that are most commonly affected. The initial symptom of ischemic necrosis is pain when the joints are being moved or bearing weight. As the condition progresses, pain is also felt when the person is at rest, especially at night time. Decreased range of motion in the joint may eventually follow. There is currently no medical treatment for this condition, but needle decompression of the bone surgically appears to retard the process. In some people with lupus, total joint replacement becomes necessary to solve the problem. Prolonged treatment with corticosteroids may also put a patient at a higher risk for development of osteoporosis. Osteoporosis, a condition in which bone mass is decreased, means that the individual is at higher risk of bone fracture and compression of vertebrae in the spine. Osteoporosis is a common problem, especially for elderly and physically inactive individuals, whether or not they have lupus or have taken steroids. Women are at a much higher risk of developing osteoporosis than men because of their smaller bone mass. The use of calcium and Vitamin D, in addition to regular exercise, may help prevent osteoporosis. A regular, well-designed exercise program is important to help prevent muscle weakness in people with lupus myositis.
Steroids In The Treatment Of Lupus Many of the symptoms of lupus result from inflammation in various tissues of the body. Cortisone, manufactured naturally by the body's adrenal glands and also made synthetically, has been found to have a marked anti-inflammatory effect. Cortisone and its derivatives are steroids, the most effective anti-inflammatory drugs known. Their use can substantially reduce the swelling, warmth, tenderness and pain that is associated with inflammation. While steroid dosage should be kept at the lowest effective level, steroids must not be stopped suddenly if they have been taken for more than four weeks. After that time, some shrinking of the adrenal glands will occur, and they may not produce enough cortisone if the synthetic steroids are discontinued abruptly. A slow reduction in the dosage of steroids allows the adrenal glands to regain their ability to manufacture natural cortisone. Prednisone and other steroids should not be stopped suddenly. Lupus patients should discuss the reasons for using steroids and other treatment alternatives which may be available with their physician. Prednisone Steroids produced by the outer part (cortex) of the adrenal gland are called "corticosteroids." Prednisone is the synthetic corticosteroid preparation most often used in the treatment of lupus. It comes in tablets of 1, 5, 10, and 20 milligrams (mg). It may be given as often as four times each day, as infrequently as once every other day, or at any frequency in between. Less than 10 mg per day is generally considered a low dose; 11 to 40 mg daily is a moderate dose; and 41 to 100 mg daily is a high dose. Steroids may also be given by intra-muscular (IM) injection or may be injected directly into a joint. Occasionally, very large doses of steroids may be given for a short period of time. This treatment, referred to as "pulse steroid treatment," involves giving 1000 mg of methyl-prednisone intravenously each day for three days. Prednisone is an extremely effective drug and may be necessary to control active lupus. Although many lupus patients do not need to stay on steroids continuously, those with severe disease or active and serious kidney lupus may require long-term steroid treatment. There is usually prompt relief of most symptoms after initiation of treatment with corticosteroids. When pleurisy or pericarditis occur, small or moderate doses of steroids are helpful. Steroids can often be avoided completely in mild cases of lupus (i.e., those involving only the joints and skin). In addition to prednisone, some other cortisone derivatives include hydrocortisone, methylprednisolone (Medrol) and dexamethasone (Decadron).
Side Effects Some of the more common side effects of steroids include changes in appearance, such as acne, development of a round or moon-shaped face, and an increased appetite leading to weight gain. Steroids may also cause a redistribution of fat, leading to a swollen face and abdomen, but thin arms and legs. In some cases, the skin becomes more fragile, which leads to easy bruising.
Kidney Disease And Lupus Lupus nephritis or lupus glomerulonephritis is the medical term for the kidney disease which occurs in systemic lupus erythematosus (SLE). It is estimated that about a third of patients with lupus will develop nephritis which requires medical evaluation and treatment. Lupus nephritis is an important and potentially serious symptom of lupus.
CLINICAL COURSE OF LUPUS NEPHRITIS There are very few signs or symptoms of lupus nephritis. It does not produce pain in the abdomen or back, nor does it cause pain or burning during urination. The loss of protein in the urine from lupus nephritis may lead to fluid retention with weight gain and swelling (edema). This may result in puffiness in the legs, ankles and/or fingers. This puffiness is often the first symptom of lupus nephritis noted by the patient. The clinical course of lupus nephritis is highly variable. Often findings of lupus nephritis are evident only in urine studies. In many patients, the urine abnormalities are very mild and may be present on one examination and absent the next. This form of lupus nephritis is rather common and, generally does not require any special medical evaluation or treatment. However, in some patients, the abnormal findings on urine studies persist or may even worsen over time. Patients with this type of lupus nephritis are at risk for loss of kidney function. They may require additional studies to evaluate the extent of their lupus nephritis and to determine the best treatment approach to control their disease. It is important to recognize that not all kidney problems in patients with lupus are due to lupus nephritis. For instance, infections of the urinary tract with burning on urination are quite common in lupus patients and require antibiotic treatment. Similarly, medications used in lupus treatment may produce signs or symptoms of kidney disease that can be confused with lupus nephritis. Salicylate compounds (e.g., aspirin), or non-steroidal anti-inflammatory drugs) are the most common type of medications used by lupus patients that can produce kidney problems. These drugs can cause loss of kidney function or fluid retention. These problems usually fade when the medications are discontinued.
STUDIES TO EVALUATE LUPUS NEPHRITIS There are a number of studies that can be done to test for kidney disease in a patient with lupus. Urinalysis. A urinalysis is by far the simplest and most commonly used study to test for lupus nephritis.
The Eye and Systemic Lupus Erythematosus Systemic Lupus Erythematosus is a wide ranging disease and can affect many organ systems, and the eye is no exception. Involvement of the eyeball itself is much more common than involvement of the orbit, or socket of the eye. However, when there is involvement of the orbit this is most often manifested by the formation of modules on the conjunctiva (the most exterior tissue layer of the eyeball and inner lid). There may also be an accompanying swelling or edema of the lids themselves. The most common observable ocular finding in lupus is the presence of "cotton wool spots" in the retina, or lining of the eye. These "spots "represent areas of the retina which are edematous due to a decreased blood flow, and hence oxygen supply, to certain areas of the retina. Of great importance to both the patient and the doctor is that these changes in the retina will often parallel exacerbations in the general disease state. Although the presence of a "cotton wool spot" is nonspecific to lupus, the presence of one in a young to middle aged patient should suggest lupus. There are other less common changes which may develop in the retina, and these include the deposition of fat cells in the retina, narrowing the arteriolar blood supply, and occlusion of the main blood vessels to the eye, which could result in a significant loss of visual acuity. Keratoconjunctivitis sicca, or the dry eye syndrome, is another problem which is often encountered in lupus patients. This is manifested by gritty sensations in the eye, decreased tears, burning and itching. Of interest is that paradoxical watering of the eyes may occur, due to the increased irritation of the eyes. This is a most annoying condition which can be helped symptomatically in a large number of patients with the proper medication. The occurrence of Keratoconjunctivitis sicca, with symptoms of dry mouth and arthritis is the symptom complex referred to as Sjogren's Syndrome. Involvement of the brain, or central nervous system, may produce blindness, atrophy of the optic nerve, nystagus (which is rocking of theeye), or even palsies of the various muscles which control the movement of the eyes. The therapy of lupus and its ocular complications is oriented toward the site of the prominent disease activity. The use of rest, salicylates (aspirin), antimalarials (such as chloroquine-aralen, resochin or Plaquenil) and steroids (cortisone) may all be quite beneficial to the lupus patient. The use of certain immunosuppressive medications is still under investigation. Prolonged therapy with chloroquine may result in pathologic changes in the lens.
|
 |
|
|
 |
 |
|||||||||||
 |
|||||||||||||
Home | Dry/Sensitive Skin | Skin Renewal | Skin Complexion & Acne | Dermatology Patient Education |